How Gynecomastia Works? Medical Explained
Ever noticed some extra “padding” in the chest area that just won’t go away, no matter how many bench presses you do? You aren’t alone.
In Malaysia, many men deal with this condition, often feeling a bit self-conscious about it. Let’s break down the science of what’s actually happening under the skin.
What Is Gynecomastia?
Medical Definition of Gynecomastia
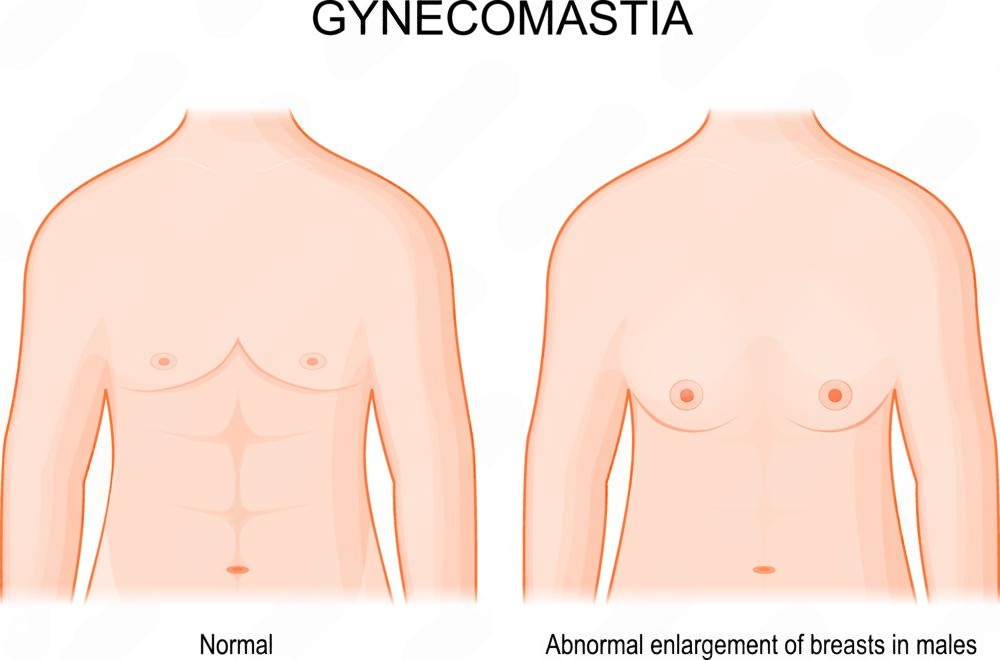
At its core, gynecomastia is the non-cancerous enlargement of male breast tissue. It’s not just “man boobs” or extra weight; it is a clinical condition where the glandular tissue—the firm stuff behind the nipple—grows due to a specific biological trigger.
Gynecomastia vs Chest Fat (Pseudogynecomastia)
It’s easy to confuse the two. Pseudogynecomastia is simply an accumulation of fat in the chest, often seen in guys carrying a few extra kilos.
However, true gynecomastia involves the growth of actual breast glands. You can usually tell the difference by touch: fat feels soft, while glandular tissue feels like a firm, rubbery lump.
How Gynecomastia Works in the Male Body
Hormonal Imbalance Between Estrogen and Testosterone
The male body produces both testosterone (the “male” hormone) and estrogen (the “female” hormone). Normally, testosterone keeps estrogen in check.
Gynecomastia happens when the balance of these hormones tips. If your testosterone levels drop or your estrogen levels spike, the breast tissue receives a signal to start growing.
How Breast Gland Tissue Develops and Enlarges
When estrogen dominates, it binds to receptors in the breast area. This stimulates the ductal structures to branch out and the surrounding stroma to thicken.
This is why the area right under the areola often feels tender, sensitive, or swollen during the early stages.
Why Gynecomastia Can Be Unilateral or Bilateral
Hormones travel through the whole body, but they don’t always affect both sides equally.
While bilateral gynecomastia affects both breasts, unilateral gynecomastia (affecting just one side) is also very common. This usually happens because one side’s tissue is simply more sensitive to hormonal signals than the other.
Biological Causes Behind How Gynecomastia Works
Puberty-Related Hormonal Changes
Puberty is a hormonal rollercoaster. Up to 60% of boys experience some form of breast swelling during their teens because their bodies are still figuring out the right testosterone-to-estrogen ratio.
Luckily, for most Malaysian teenagers, this usually settles down on its own within a year or two.
Age-Related Hormonal Decline
As men get older, testosterone levels naturally begin to dip. At the same time, body fat often increases, and fat cells actually convert testosterone into estrogen.
This “double whammy” makes gynecomastia in older men quite common as the hormonal gap widens.
Medical and Metabolic Triggers
Sometimes, it isn’t just age or puberty. Certain medications—like some anti-anxiety meds, hair loss treatments, or steroids—can disrupt how the body processes hormones.
Additionally, underlying issues with the liver or kidneys can lead to unwanted growth.
Types of Gynecomastia and How Each Works
Glandular Gynecomastia
This is “true” gynecomastia. It is characterized by firm, fibrous tissue directly under the nipple. It is strictly caused by the growth of the breast gland itself rather than weight gain.
Fat-Dominant Gynecomastia
Mostly seen in men with higher BMIs, this type is primarily composed of adipose (fat) tissue. While it looks like gynecomastia, there is very little actual glandular tissue present upon examination.
Mixed Gynecomastia
This is the most common type we see in clinics. It’s a combination of both excess fat and enlarged glandular tissue. To fix this, both the fat and the gland usually need to be addressed simultaneously.
How Gynecomastia Progresses Over Time
Early Development Stage
In the first 6 to 12 months (the florid phase), the tissue is actively growing. This is often the stage where guys experience pain or a “burning” sensation in the chest.
Stable and Fibrotic Stage
If the hormonal issue isn’t fixed, the tissue becomes “fibrotic.” The soft, growing gland turns into tough, scarred tissue.
At this point, the American Society of Plastic Surgeons notes that the growth is likely permanent and won’t shrink with diet or exercise alone.
How Gynecomastia Is Clinically Diagnosed
Physical and Hormonal Assessment
A doctor will start with a physical exam to feel the consistency of the tissue. They may also order blood tests to check your testosterone, estrogen, and thyroid levels to rule out underlying health issues.
Imaging to Confirm Glandular Enlargement
In some cases, an ultrasound or mammogram is used to get a clear picture of what’s inside. This helps the doctor confirm if it’s fat, a gland, or in very rare cases, something more serious that requires attention.
How Gynecomastia Resolves or Persists
Natural Regression vs Permanent Tissue Growth
If the cause is puberty, the tissue usually disappears within six months to two years. However, if the tissue has been there for more than a year and has become fibrotic, it rarely goes away on its own.
Factors That Influence Reversibility
Several things determine if the condition will reverse:
Duration: The longer it’s there, the more “set” the tissue becomes.
Cause: If it’s caused by a medication you’ve stopped, it might shrink.
Lifestyle: Reducing alcohol and avoiding certain supplements can help prevent it from worsening.
How Treatment Targets the Mechanism of Gynecomastia
Medical Management Based on Hormonal Cause
If caught very early, doctors might prescribe Selective Estrogen Receptor Modulators (SERMs) like Tamoxifen.
These drugs block estrogen from “talking” to the breast tissue, potentially halting the growth before it becomes permanent.
Surgical Correction of Glandular Tissue
For most men, the gold standard is surgery. This involves liposuction to remove the fat and a small incision to physically excise the firm gland.
Since the gland is removed, the results are typically permanent. If you’re curious about the specific surgical techniques used today, you can find more details at WebMD.
