If you’ve been scrolling through social media or chatting with friends about the latest “tweakments,” you’ve likely heard of PRP treatment. Whether it’s called the “Vampire Facial” or a miracle for thinning hair, Platelet-Rich Plasma (PRP) has become a staple in Malaysia’s aesthetic and medical scene. It’s natural, it’s versatile, and it uses your own body to do the heavy lifting.
GLOJAS Specialist Clinic offers premier PRP treatments in Malaysia, utilizing advanced hair restoration and skin rejuvenation techniques to deliver natural, long-lasting results for every patient.
What Is PRP Treatment?
At its core, PRP treatment is a regenerative therapy that uses a concentrated version of your own blood to speed up healing and stimulate growth. Because it is autologous (meaning it comes from you), the risk of allergic reactions is virtually zero. It’s essentially “liquid gold” for your skin, hair, and joints.
How PRP Treatment Works
The magic isn’t in a synthetic chemical; it’s in your blood’s innate ability to repair itself.
PRP Mechanism: Platelets & Growth Factors
Your blood contains platelets, which are famous for clotting but even better at healing. When concentrated, these platelets release growth factors that act like messengers, telling your cells to produce more collagen, repair damaged tissue, and improve blood circulation in the treated area.
Procedure Steps: What to Expect
Blood Draw: A small amount of blood (similar to a routine lab test) is taken from your arm.
Centrifugation: The blood is placed in a centrifuge machine that spins at high speeds to separate the plasma from the red blood cells.
Activation: The golden, platelet-rich plasma is collected.
Injection: The PRP is carefully injected or microneedled into the target area (scalp, face, or joint).
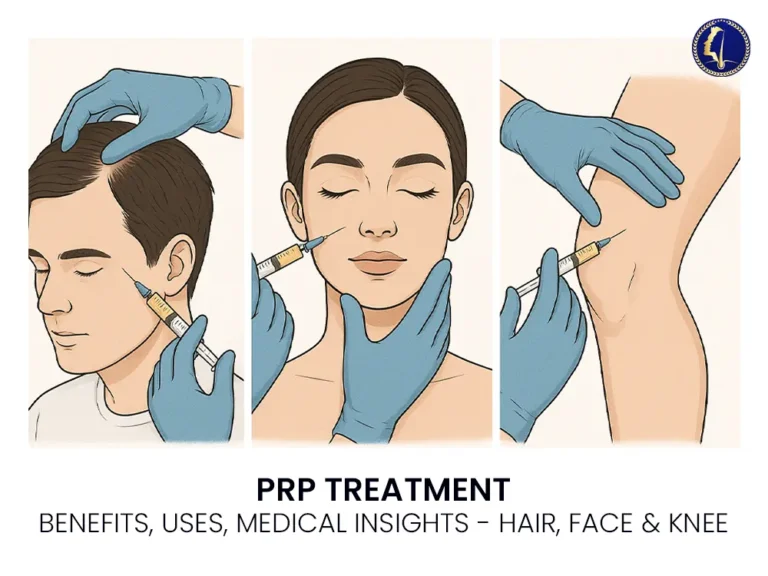
Types of PRP Treatment
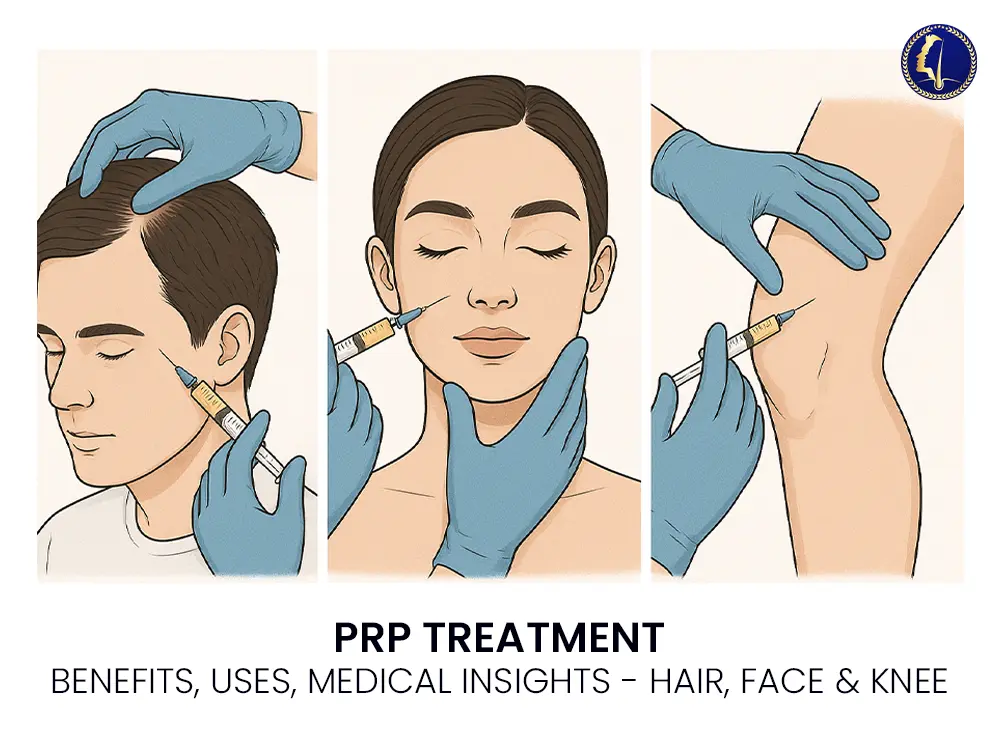
In Malaysia, PRP isn’t just a one-trick pony. It’s widely used across three main categories:
PRP for Hair Loss
This is a game-changer for those dealing with androgenetic alopecia or general thinning. By injecting PRP into the scalp, the growth factors wake up dormant hair follicles, leading to thicker, healthier strands.
PRP for Skin Rejuvenation
Often paired with microneedling, this treatment—popularized as the Vampire Facial—targets fine lines, acne scars, and dullness. It’s a favorite for those seeking a natural glow-up without synthetic fillers.
PRP for Joint Pain & Orthopedic Use
Athletes and those with osteoarthritis often turn to PRP to manage knee or joint pain. It helps reduce inflammation and can potentially slow down cartilage degeneration.
Benefits of PRP Treatment
Why is everyone in KL and Penang talking about this? Because the results are backed by biology.
Improved Healing & Tissue Regeneration
Whether it’s a sports injury or a stubborn acne scar, PRP accelerates the body’s repair timeline. It’s often used post-surgery to help tissues knit back together faster.
Hair Growth & Thicker Hair
Unlike topical solutions that you have to apply every single day, PRP works at the follicle level. Many patients see a significant reduction in hair fall and an increase in hair density after a few sessions.
Younger, Firmer Skin
By boosting collagen and elastin, PRP helps tighten sagging skin and smooth out those pesky “smile lines.”
Risks & Side Effects
While PRP is very safe, it’s still a medical procedure.
Common Mild Reactions
Swelling and Redness: Usually subsides within 24–48 hours.
Bruising: Small bruises at the injection site are common but temporary.
Tenderness: The area might feel a bit sore for a day or two.
Rare Complications
Though rare, if the procedure isn’t done in a sterile environment, there is a small risk of infection or nerve injury. This is why choosing a certified medical clinic is non-negotiable.
PRP Treatment Cost in Malaysia
Let’s talk numbers. The cost of PRP can vary quite a bit depending on where you go and what you’re treating.
Price Range by Clinic
On average, a single session of PRP in Malaysia costs between RM 1,000 and RM 3,500.
Hair Loss: RM 1,500 – RM 3,000 per session.
Facial Rejuvenation: RM 1,200 – RM 2,800 per session.
Joint Injections: RM 2,000 – RM 4,500 per session.
Factors Affecting Cost
Clinic Location: Expect to pay more in prime areas like Bangsar or Bukit Bintang.
Doctor’s Expertise: Specialist dermatologists or orthopedic surgeons often charge higher fees than general aesthetic doctors.
Technology Used: Some clinics use advanced kits that produce a higher concentration of platelets, which can increase the price.
Choosing the Right PRP Clinic in Malaysia
Don’t just go for the cheapest “groupon” deal you find. Your safety comes first.
Certifications & Experience
Ensure the clinic is registered with the Ministry of Health (MOH) and the doctor holds a valid Letter of Credentialing and Privileging (LCP) for aesthetic medical practice.
Patient Reviews & Before-After Results
Check Google reviews and ask to see real “before and after” photos of previous patients. A reputable clinic will be transparent about the results you can realistically expect.
PRP Treatment FAQs
How Long Do Results Last?
For skin and hair, results typically last 6 to 18 months. Maintenance sessions once or twice a year are usually recommended to keep the glow (or the hair) going.
Is PRP Painful?
It’s more “uncomfortable” than painful. Most clinics apply a topical numbing cream before the injections to make the process as breezy as possible.
How Many Sessions Do You Need?
Most experts recommend an initial series of 3 to 6 sessions, spaced about 4 weeks apart, for optimal results.
Conclusion: Is PRP Treatment Right for You?
If you’re looking for a natural, low-risk way to tackle hair thinning, skin aging, or joint discomfort, PRP is a fantastic option. It’s not an “instant fix,” but for those who value long-term health and natural-looking results, it’s worth the investment.