Hair Loss
Hair loss is a common yet often distressing condition that affects millions of men and women worldwide. While it can be a natural part of aging, it may also indicate underlying health issues, lifestyle factors, or genetic predispositions. Understanding the types, causes, and evidence-based treatment options for hair loss is essential for effective management.
This comprehensive guide provides a medically sound overview of hair loss, combining clinical insights with practical strategies for patients and healthcare professionals.
What is Hair Loss?

Hair loss, medically known as alopecia, refers to the partial or complete loss of hair from areas where it normally grows. It can be temporary or permanent, affecting the scalp, eyebrows, eyelashes, or other parts of the body.
Hair loss is not a diagnosis in itself, but a symptom of various conditions, ranging from hormonal imbalances to autoimmune disorders and dermatological diseases.
Common Types of Hair Loss
Understanding the type of hair loss is the first step toward accurate diagnosis and treatment:
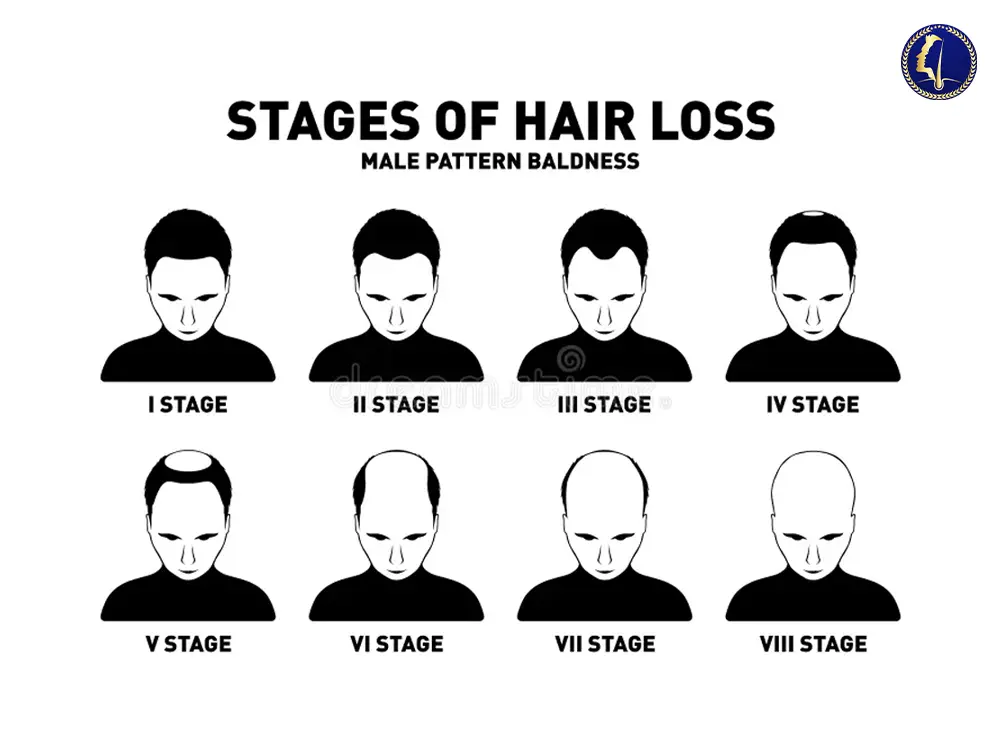
1. Androgenetic Alopecia
Also known as male or female pattern baldness, this is the most common form and is genetically inherited. In men, it often presents as a receding hairline and vertex thinning. In women, it usually causes diffuse thinning at the crown.
2. Telogen Effluvium
This is a temporary condition often triggered by stress, surgery, childbirth, or nutritional deficiencies. It results in diffuse shedding due to a disruption in the hair growth cycle.
3. Alopecia Areata
An autoimmune disorder where the immune system mistakenly attacks hair follicles, leading to patchy bald spots. It may progress to total scalp (alopecia totalis) or body hair loss (alopecia universalis).
4. Traction Alopecia
Caused by physical stress on hair follicles, such as tight hairstyles or extensions, this type of alopecia is preventable and often reversible in early stages.
5. Scarring Alopecia
This irreversible condition involves inflammation that destroys hair follicles and replaces them with scar tissue. Early detection by a dermatologist is critical.
Medical Causes of Hair Loss
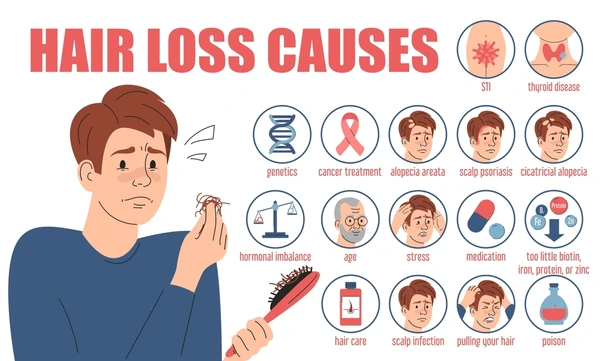

Hair loss can stem from several systemic and localized medical conditions, including:
Hormonal imbalances (e.g., thyroid disease, PCOS)
Nutritional deficiencies (iron, vitamin D, biotin, zinc)
Autoimmune conditions (e.g., lupus, alopecia areata)
Infections (e.g., tinea capitis or scalp ringworm)
Medications (chemotherapy, anticoagulants, beta-blockers)
Chronic stress or trauma
Rapid weight loss or eating disorders
Proper medical evaluation, including blood tests, scalp biopsy, and trichoscopy, helps determine the underlying cause and rule out serious health issues.
Evidence-Based Treatment Options
🔹 Topical Treatments
Minoxidil (Rogaine): FDA-approved for both men and women, it promotes hair regrowth by extending the anagen (growth) phase.
Corticosteroids: Used topically or injected for autoimmune-related hair loss.
🔹 Oral Medications
Finasteride (Propecia): Inhibits DHT, a hormone implicated in androgenetic alopecia (only for men).
Spironolactone: Off-label use in women with hormonal hair loss due to its anti-androgen effects.
🔹 Non-Pharmacological Therapies
Platelet-Rich Plasma (PRP): Involves injecting autologous platelets into the scalp to stimulate hair growth.
Low-Level Laser Therapy (LLLT): Improves hair density through photobiomodulation.
Microneedling: Enhances the absorption of topical treatments and stimulates collagen production.
🔹 Hair Transplant Surgery
For advanced cases of androgenetic alopecia, follicular unit transplantation (FUT) or follicular unit extraction (FUE) provides permanent restoration with natural-looking results.
Preventive Strategies and Lifestyle Modifications
While not all types of hair loss are preventable, certain lifestyle practices can support scalp health:
Balanced nutrition rich in iron, protein, and essential vitamins
Stress management through mindfulness or cognitive behavioral therapy
Gentle hair care: Avoid harsh chemicals, excessive heat, and tight hairstyles
Regular scalp hygiene to prevent folliculitis and fungal infections
When to See a Doctor
You should consult a board-certified dermatologist if you experience:
Sudden or rapid hair loss
Bald patches or clumps of hair falling out
Scalp itching, pain, or inflammation
Hair loss following a new medication or illness
Family history of genetic hair loss
Early diagnosis often leads to better outcomes and prevents irreversible damage to hair follicles.
5 Frequently Asked Questions (FAQs)
1. Is hair loss reversible?
It depends on the cause. Telogen effluvium and early-stage androgenetic alopecia are often reversible, especially with prompt intervention. Scarring alopecia is usually permanent.
2. Does stress really cause hair loss?
Yes. Chronic stress can disrupt the hair growth cycle, leading to telogen effluvium. Managing stress may reduce shedding over time.
3. Are natural remedies effective for hair regrowth?
While some natural oils (like rosemary or pumpkin seed oil) have shown modest results, evidence-based treatments like minoxidil or PRP offer more consistent outcomes.
4. How long before treatments show results?
Most treatments take 3–6 months to show visible improvement. Hair growth is slow and requires patience and consistent use.
5. Can frequent washing or shampooing cause hair loss?
No. Washing helps maintain scalp health. However, harsh shampoos or overuse of heat styling tools can damage hair shafts and lead to breakage.
Final Thoughts: Take a Proactive Approach to Hair Loss
Hair loss is multifactorial and often emotionally challenging, but it is manageable with the right medical guidance. Whether due to genetics, stress, or underlying disease, timely diagnosis and evidence-based treatment can restore both hair density and patient confidence.
For the best results, always seek a board-certified dermatologist or trichologist who can offer a personalized treatment plan backed by clinical data

