Gynecomastia
Gynecomastia is a benign condition characterized by the enlargement of male breast tissue. Although it is often underreported due to social stigma, gynecomastia is relatively common, affecting an estimated 30–70% of males at some point in their lives. This article provides a medically accurate, comprehensive overview of gynecomastia, integrating current clinical understanding and evidence-based treatment approaches.
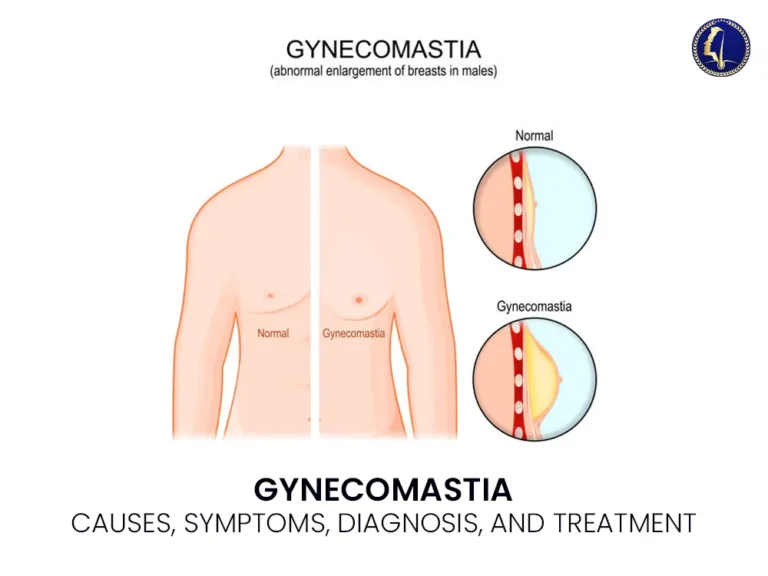
What Is Gynecomastia?
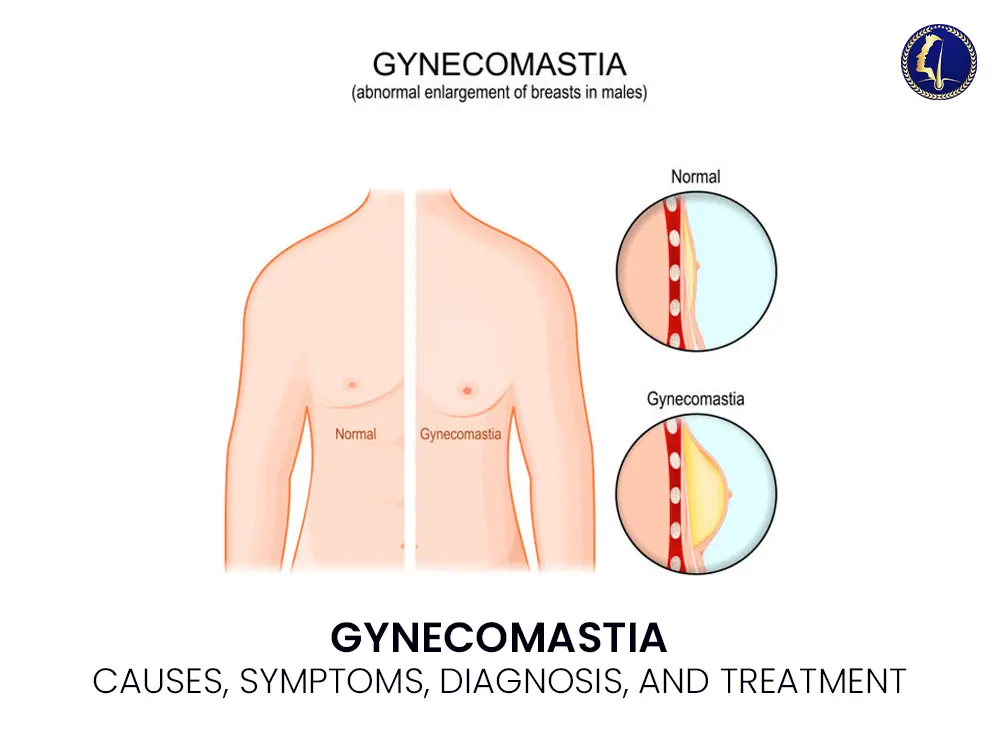
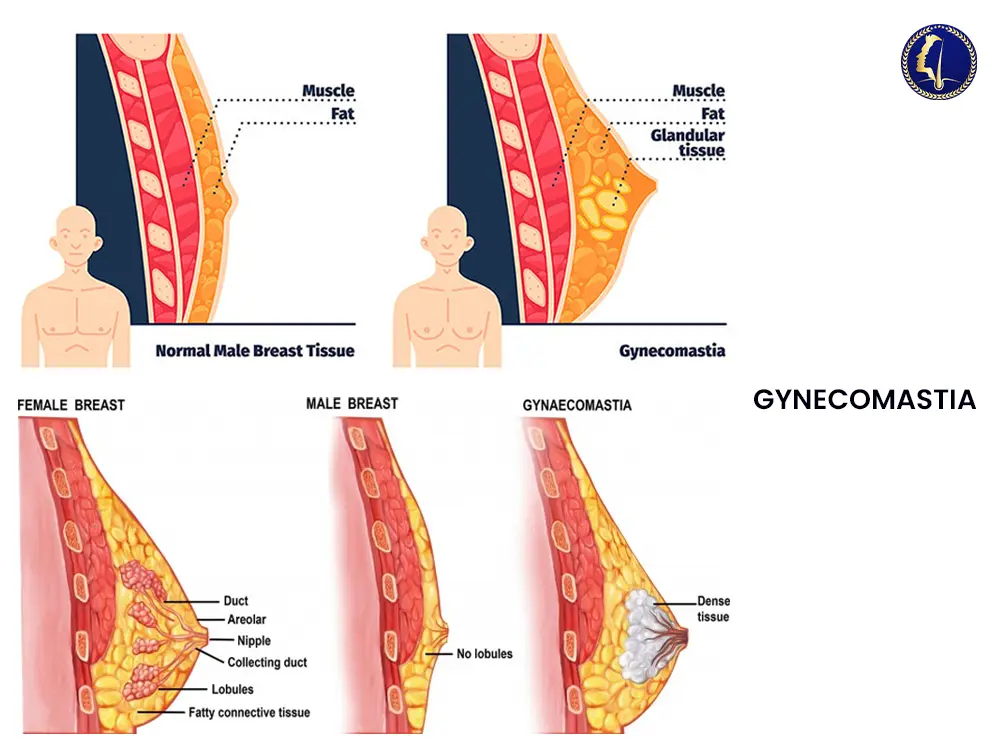
Gynecomastia is defined as the proliferation of glandular breast tissue in males. It differs from pseudogynecomastia, which involves fat accumulation without glandular proliferation, typically due to obesity. The condition may affect one or both breasts and can occur at various life stages, including infancy, puberty, and older adulthood.
The underlying mechanism often involves an imbalance between estrogen and androgen activity. Estrogen stimulates breast tissue growth, whereas androgens (such as testosterone) counteract this effect. An excess of estrogen or a relative deficiency of testosterone can disrupt this balance, leading to breast tissue enlargement.
Etiology: What Causes Gynecomastia?
The causes of gynecomastia are diverse and may be physiological, pharmacological, or pathological.
1. Physiological Causes
Neonatal gynecomastia: Due to maternal estrogen transfer, this resolves spontaneously.
Pubertal gynecomastia: Common in adolescent males, usually transient and self-limiting.
Senile gynecomastia: Occurs in older men due to declining testosterone levels and increased aromatase activity converting androgens to estrogens.
2. Pharmacological Causes
A wide array of medications has been implicated, including:
Antiandrogens (e.g., spironolactone, flutamide)
Anabolic steroids
Antipsychotics (e.g., risperidone)
Antidepressants
Calcium channel blockers
Proton pump inhibitors
HIV medications (e.g., efavirenz)
The risk increases with chronic use and higher dosages.
3. Pathological Causes
Hypogonadism (primary or secondary): Klinefelter syndrome, testicular failure
Liver disease: Cirrhosis impairs estrogen metabolism
Chronic kidney disease
Tumors: Testicular, adrenal, or pituitary tumors
Hyperthyroidism
Symptoms and Clinical Presentation
Gynecomastia typically presents as:
Palpable, rubbery or firm mass beneath the nipple
Symmetrical or asymmetrical breast enlargement
Tenderness or discomfort in some cases
Psychological distress or embarrassment
Unlike breast cancer, which is rare in males, gynecomastia tissue is usually central, bilateral, and lacks skin dimpling or nipple discharge.
Diagnosis: Clinical and Investigative Approach
History and Physical Examination
A detailed clinical history should assess:
Onset and duration
Pubertal stage (in adolescents)
Drug and supplement use
Signs of systemic disease
The physical exam should include breast palpation, testicular exam, and assessment for signs of liver or thyroid dysfunction.
Laboratory Investigations
Blood tests may be ordered to rule out endocrine disorders:
Serum testosterone, estradiol, LH, FSH
Liver and kidney function tests
Thyroid function tests
Beta-hCG and alpha-fetoprotein (to rule out testicular tumors)
Imaging
If malignancy is suspected or if the presentation is atypical:
Ultrasound of the breast
Mammography (in older males or high-risk cases)
Testicular ultrasound if tumors are suspected
Differential Diagnosis
It is essential to differentiate gynecomastia from:
Pseudogynecomastia
Male breast cancer
Lipoma
Breast abscess or cyst
Accurate diagnosis is crucial to guide appropriate treatment and to avoid unnecessary anxiety or interventions.
Treatment Options
Treatment depends on the underlying cause, the severity, and the duration of the condition.
Observation and Reassurance
For physiological gynecomastia in adolescents or cases related to reversible drug use, watchful waiting is appropriate. Reassurance is often sufficient, especially if the tissue is non-tender and has developed within the past six months.
Medical Therapy
In persistent or painful gynecomastia, pharmacologic treatment may be considered:
Selective Estrogen Receptor Modulators (SERMs) like tamoxifen or raloxifene
Aromatase inhibitors (less effective and rarely used)
Testosterone replacement therapy (in hypogonadal men)
Note: Medical therapy is most effective if initiated within the first year of breast tissue development.
Surgical Management
Indicated in chronic, large, or fibrotic gynecomastia or when conservative measures fail. Surgical options include:
Subcutaneous mastectomy
Liposuction-assisted mastectomy
Minimally invasive endoscopic techniques
Outcomes are generally favorable with high patient satisfaction and low recurrence rates.
Psychological Impact and Patient Counseling
Beyond physical symptoms, gynecomastia can lead to:
Social withdrawal
Low self-esteem
Depression or anxiety
Clinicians should approach the condition with sensitivity, empathy, and clinical judgment. Involving a psychologist or counselor can be beneficial, especially for adolescents.
Prognosis
The prognosis of gynecomastia is generally excellent. Most cases resolve with conservative management, especially those related to puberty or medication. Surgical outcomes are typically long-lasting and cosmetic results are satisfactory.
Conclusion
Gynecomastia is a benign yet potentially distressing condition that warrants a thoughtful, evidence-based approach. Accurate diagnosis, patient-centered counseling, and tailored therapy options—from observation to surgery—form the cornerstone of management.
With growing awareness and reduced stigma, more men are seeking help and receiving effective treatment for gynecomastia, improving both their physical and psychological well-being.
Frequently Asked Question – Gynecomastia
1. What is gynecomastia and what causes it?
Gynecomastia is the enlargement of male breast tissue due to hormonal imbalance, often from increased estrogen or decreased testosterone levels.
2. How do I know if I have gynecomastia or just fat?
Gynecomastia involves firm, glandular tissue under the nipple, while fat accumulation (pseudogynecomastia) feels soft and is usually due to obesity.
3. Can gynecomastia go away on its own?
Yes, gynecomastia can resolve without treatment, especially during puberty or if caused by reversible drug use. Persistent cases may need therapy or surgery.
4. What are the treatment options for gynecomastia?
Treatment includes observation, hormone therapy (like tamoxifen), or surgical options such as subcutaneous mastectomy or liposuction.
5. Is gynecomastia dangerous or a sign of cancer?
Gynecomastia itself is benign. However, rare cases of male breast cancer should be ruled out if there is rapid growth, nipple discharge, or asymmetry.